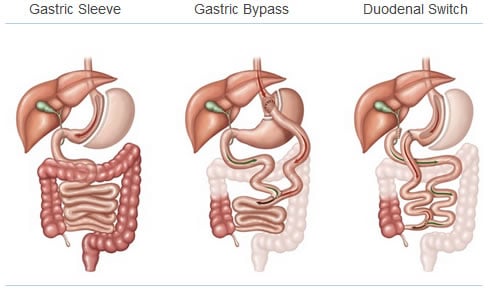
If you have ever researched the term "weight loss" or "bariatric surgery", you have probably heard about the gastric bypass or sleeve gastrectomy. However there is another successful weight loss procedure that is not as common, known as the biliopancreatic diversion with duodenal switch. Over the last several months, I have posted details about the other commonly performed weight loss surgeries. In this blog post today, I will detail the science behind the biliopancreatic diversion with duodenial switch.
The biliopancreatic diversion with duodenal switch, BPD-DS, is the least commonly performed bariatric surgical procedure. However, as patients and practicing physicians are learning more about this procedure, it is becoming more popular.
The doudenal switch is a combination of the sleeve gastrectomy and the gastric bypass. The biliopancreatic diversion with duodenal switch, commonly referred to as the duodenal switch (DS), statistically has the best overall weight loss results despite the frequency at which it is performed. On average, patients routinely lose 80% of their excess weight and in many cases, closer to 100%.
So if the duodenal switch has the best overall weight loss results, then why doesn't everybody have this procedure? In our practice we tend to reserve the duodenal switch for our heavier patients who need to maximize their weight loss. Below, I will also explain a few other reasons why patients may choose different procedures over the DS.
Before reading, review these terms for a better understanding.
1. Biliopancreatic diversion with duodenal switch – A surgical weight loss procedure that involves performing a sleeve gastrectomy and also rerouting the small intestine in a manner similar to the gastric bypass.
2. Jejunum – The middle part of the small intestine below the duodenum.
3. Ileum –The lower 1/3 of the small intestine.
4. Duodenum – The first and shortest part of the small intestine that aids in the absorption of food.
5. Malabsorption – A condition in which the small intestine can not absorb all the nutrients from the food consumed.
6. Pancreaticobiliary Limb – A limb of the intestine that carries digestive juices; there is no food contained in this limb of intestine.
7. Alimentary Limb – A limb of the intestine that carries the food; there is no digestive juices in this segment of intestine.
8. Common Channel – This is a limb of intestine that contains both food can digestive juices. This is the segment of the small intestine that is primarily responsible for the absorption of nutrients
9. Laparoscopic – A method of surgery that creates small incisions in the abdomen and is performed using a camera. This type of procedure is also known as minimally invasive surgery.
How it Works:
In performing the duodenal switch, the surgeon creates a sleeve gastrectomy as previously detailed. Additionally the duodenum, which is the first part of the small intestine, is divided. The surgeon then identifies the end of the small intestine were it is attached to the colon and measures back about 5 feet This area is marked and then the surgeon measures back another 5 feet or so. At this site, about 10 feet from the colon, the small bowel is divided and this part of the small intestine where the division occurs is reconnected to the duodenum/stomach and also the small bowel is reconnected to establish intestinal continuity about 5 feet from the colon.
Ultimately, the duodenal switch removes part of the stomach and significantly shortens the small bowel from a digestive/absorptive standpoint. This results in smaller portions of food consumed and faster movement of those portions through your digestion system.
 The New Way of Digestion.
The New Way of Digestion.
The duodenal switch works to create a small stomach, essentially a sleeve gastrectomy, about the size of a banana, that is then connected directly to the lower 1/3 of of the small intestine (ileum). As a result, the rest of the upper portion of the small intestine (duodenum and jejunum) is bypassed.
More specifically, In this altered anatomy, food travels down the "new" portion of the stomach and enters the small intestinal segment called the ileum (the alimentary/enteric limb). Digestive juices are then released from the liver and the pancreas, traveling down the pancreaticobiliary limb. The food and the digestive juices meet about 5 feet from the colon and are absorbed within the common channel.
In a similar manner to the gastric bypass, the small intestine is also shortened in the DS (however much shorter then the bypass), therefore there is less absorption of nutrients. Duodenal switch patients may experience greater changes in mineral deficiencies and bowel function compared to a gastric bypass patient. Therefore it is extremely important for these patients to get adequate nutritional intake in the form of protein and nutritional supplements to ensure they are receiving the appropriate amount of vitamins and minerals to sustain a healthy lifestyle.

Unlike the gastric bypass, which the small intestine is shortened by about 25 – 30%, the duodenal switch bypasses in excess of 75% of the small intestines absorptive capacity. As a result of this, the duodenal switch is considered a malabsorptive operation, which makes the likelihood of nutritional deficiencies and changes in bowel function much higher. Because of these extreme alterations to the body’s method of digestion, our practice mostly reserves the duodenal switch for our patients who have a much higher body mass index, usually 55 or higher. Although this operation can be performed on lower body mass indexes, patients who have the sleeve gastrectomy or the gastric bypass can still expect a significant amount of weight loss with a lower nutritional risk.
The obvious benefit of the duodenal switch is weight loss.
Traditionally, surgeons would claim that weight loss surgery was effective because it resulted in eating less (restriction) and absorbing fewer calories (malabsorption). Although this is true, there are more important mechanisms as to why patients lose weight following bariatric surgeries.
Based on current research, physicians and educators believe that weight loss as a part of a duodenal switch and gastric bypass surgery is a result of bypassing the duodenum coupled with changes in a patient’s hormone levels. Indirect evidence of these hormonal changes has been recorded as a result of most gastric bypass patients with diabetes now having normal glucose control (cure of the diabetes) prior to even losing weight.
![]()
The future of bariatric surgery surgery is much safer.
In the past, bariatric surgery was performed by creating a large incision. Not only is this unappealing, but doing an open operation carries more surgical risk.
Currently, all of these weight loss operations are performed laparoscopically (TV camera surgery) or even with the surgical robot. As bariatric surgeries have evolved, so has the risk of surgery. Many patients who know they need to lose weight are afraid to consider the option of weight loss surgery because of the perceived risk. However, a laparoscopic gastric bypass has less risk then many other commonly performed abdominal surgeries. Think about that.
I always encourage our bariatric patients to consider the condition of obesity as a chronic disease. Like any other medical problem or chronic disease, it must be treated. There are multiple treatment options and surgery is one part of curing the disease of obesity.
To learn more about losing weight and your surgical options, schedule a time to come to one of our seminars








