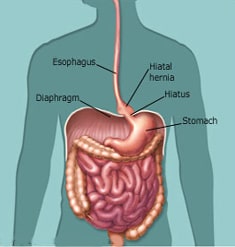
If you have ever researched bariatric surgery, you have probably heard the term "hiatal hernia." A hiatal hernia occurs when part of the stomach slides into the chest through a hole in the diaphragm called the hiatus. When this happens, it places the stomach in an unnatural position, causing a range of problems from reflux (heartburn), to chest pain and vomiting.
 The size of the hernia does not affect the severity of symptoms. Some patients may be very symptomatic with a small hernia, while others with a large hernia can have little-to-no symptoms.
The size of the hernia does not affect the severity of symptoms. Some patients may be very symptomatic with a small hernia, while others with a large hernia can have little-to-no symptoms.
Hiatal Hernia and Obesity
You may be wondering why the term "hiatal hernia" is a common medical concern within the bariatric field. Well, morbidly obese patients are at a higher risk of developing a hiatal hernia.
Hiatal hernia development is due to weakened muscle tissue that allows the stomach to bulge up through your diaphragm. Patients who carry around excess weight experience an increase in intraabdominal pressure. Yet, aside from weight gain being one of the most common reasons people develop a hiatal hernia, heavy lifting and genetics can also play a role in the development.
Similarly, patients who experience weight regain after bariatric surgery can have the recurrence or even initial development of a hiatal hernia. And the development of a hiatal hernia after bariatric surgery will act the same way—causing reflux, chest pain, and in some cases, vomiting.
Depending on the type of bariatric procedure the patient had, the symptoms of a hiatal hernia may vary in intensity and type. For example, patients who have gastric sleeve surgery may have more problems than a patient who has the gastric bypass with the primary symptom being reflux (heartburn). Patients who experience reflux after gastric sleeve surgery almost always have more severe and hard-to-manage symptoms than patients who have a gastric bypass.
However, gastric bypass patients may still experience some heartburn and vomiting if they have a hiatal hernia.
Diagnosing a Hiatal Hernia
Hiatal hernias are diagnosed in several different ways, with the most common diagnostic tests being an EGD and an Upper GI. An EGD involves passing a long flexible tube with a camera at the end of it down the esophagus into the stomach to examine the health of the upper gastrointestinal tract. Meanwhile, an Upper GI consists of swallowing a contrast material and taking X-Rays to see the anatomy of the esophagus and stomach.
As a bariatric patient going through the steps to surgery, your surgeon will perform an EGD to look for any signs of a hiatal hernia and other upper gastrointestinal tract concerns. If a hiatal hernia is found, your surgeon can correct this at the time of your bariatric surgery.
Treating a Hiatal Hernia
Initial treatment of a hiatal hernia includes changing your eating habits and any medications that may be contributing to the bulging of your stomach into the esophagus. Your surgeon will also recommend that you avoid late-night snacking and try to sleep with your head elevated.
In some cases, if you are not already planning to have bariatric surgery soon or if these treatments are not enough, surgery may be needed to repair the hernia and bring the stomach (sleeve or pouch) back into the right place.
Suppose you have already had bariatric surgery and have been diagnosed with a hiatal hernia or experience a recurrent hernia. In that case, your bariatric surgeon may recommend a complete revision of the gastric sleeve to the bypass to control symptoms and decrease the risk of recurrence of the hernia.
Once a hiatal hernia has been diagnosed, it can not be reversed without surgery. Although a hiatal hernia is manageable to live with should symptoms not be severe, chronic reflux that can not be controlled medically could lead to esophageal cancer as a result of acid damage.
If you are experiencing pain in the upper abdomen or chest, acid reflux, or vomiting, reach out to your bariatric surgeon to schedule and EGD or Upper GI. Your surgeon will be able to diagnosis you and provide you with the best treatment plan based on your health.