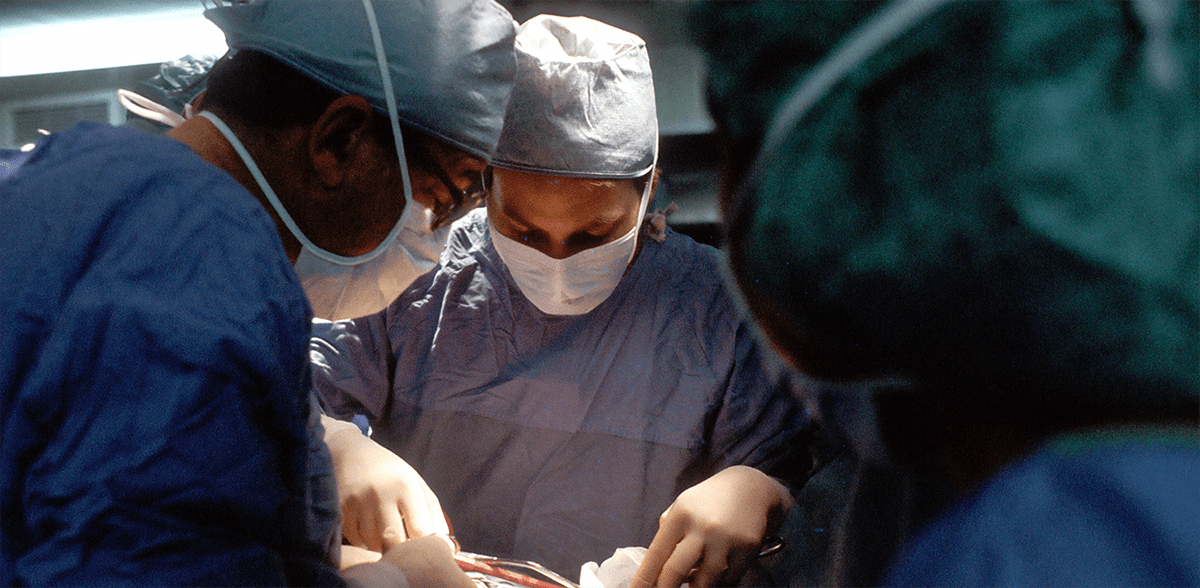
In previous blogs I’ve talk about the duodenal switch, the gastric bypass, and the gastric sleeve. Today I want to summarize these different operations and talk about what I tell my patients when they come to see us about weight loss surgery.
First off, let’s talk about the gastric sleeve. This operation we started to do in the field of weight loss surgery around 10 years ago and it has gained a lot of popularity over the last several years. In our practice it probably accounts for about 40 to 50% of the procedures that we do. This procedure is a relatively simple technical operation, where we remove about 80 to 90% of the stomach volume leaving the stomach as a small narrow tube.
In effect, what we have done is reduce is the volume of the stomach so a patient eats significantly less. But we also believe that hormones are in play that reduce hunger—so the patient feels much less hunger than they previously did before. As a result of these two effects, reduced volume of food in an early sense of satiety, along with decreased hunger, patients tend to have fairly significant weight loss. I tend to tell my patients that they will lose about 10 to 20% less weight loss than they typically will with the gastric bypass.
Moving on to the gastric bypass, this really has been the mainstay procedure that we have done in the field of weight loss surgery for many, many decades—going back to the 1980s. This probably is the operation that we have the greatest experience with, knowing about it short and long-term weight loss effects.
The gastric bypass involves creating a small pouch out of the stomach and rerouting the small intestine up to that pouch. Effectively what we’ve done with this operation is bypass the main part of the stomach to divert food away from the duodenum, which is the first part of the small intestine. Therefore, the digestive process begins further downstream; probably somewhere in the 20 to 30% range. So effectively what we’ve done is shorten the small intestine by about 20 to 30% and also made the stomach smaller so that when we eat we have a much earlier sense of satiety.
I tell my patients that the weight loss effects probably have more to do with some of the hormonal effects that we believe are occurring. Certainly patients eat significantly less as a result of the operation but by bypassing the first part of the duodenum, we believe that we are altering hormones that regulate our metabolism. Thereby, resulting in significant weight loss. Typically I would expect most of our patients lose somewhere in the 60 to 80% excess weight loss range with this operation.
The duodenal switch is an operation less commonly performed and in our practice probably about 10% of patients receive this operation. The easiest way to look at this procedure is to think of a sleeve gastrectomy along with the gastric bypass. We do the sleeve, like was previously described in earlier blogs that I’ve written about, and we also bypass the duodenum like we do with the gastric bypass.
But instead of bypassing somewhere in the neighborhood of 20 to 30% of the small intestine, we’re bypassing an excess of 70 to 80% of the small intestine. So the duodenal switch not only has all of the benefits of the sleeve gastrectomy and the gastric bypass, but there is also significant malabsorption.
And although one might think that this would be a good thing, it certainly does have some side effects. Nutritional deficiencies are much more likely to occur after the duodenal switch and there are fairly significant changes in the bowel pattern.
So what you might be asking yourself is why would we do this procedure. Well typically I would look to this operation as a potential choice for our patients who are in the heavier weight range.
So to summarize, when I see a patient for the first time and we’re talking about the various different procedures and what might be more or less effective for them, I tend to look at two things; number one what are the medical problems the patient is suffering from and also what range weight are they starting at. So to generalize, if a patient is in the lower weight range and does not have significant ongoing medical co-morbidities, like diabetes and hypertension, I tend to lean more to the sleeve gastrectomy.
For patients more in, what I would consider the middle-weight range, maybe somewhere with a body mass index in the mid-to-upper 40s and lower 50s range, or particularly with patients who suffer from diabetes where they may be taking multiple injectable type medications, I would lean more to the gastric bypass.
And then for our patients who are in the heavier weight range, and I would consider those people to be in the body mass index range of 55 and particularly above 60, I tend to direct direct those individuals to the duodenal switch. And the reason being is that for our heavier patients, although they will have significant weight loss with the sleeve and the gastric bypass, they may not achieve the degree of weight loss that we would like to see—whereby they would reduce their body mass index to a more medically acceptable range (typically under a body mass index of 40). But it is just not statistically likely that those patients in the upper body weight ranges with body mass indices above 60 are probably going to achieve that degree of weight loss with a gastric bypass or a sleeve. Now, it’s not to say that doesn’t happen, and it certainly does occur quite frequently, but just as a statistical matter a fair number of people will not achieve that degree of weight loss. Thereby in my practice I start to look toward a duodenal switch for these individuals.
Certainly there is a lot more to know about these operations. When a patient comes to see us in our practice and they go through the initial consultation and education process, we get into much greater detail about all of the procedures. We encourage any individual that is suffering from weight-related medical problems to at least seek some treatment. This doesn’t necessarily have to involve surgery, but certainly should be directed towards an aggressive medical weight loss program. And if it’s felt that a surgical approach is an option for that patient, seeing a competent bariatric surgeon who is at a center of excellence designated facility would be something that that you should certainly get more information about. Therefore you can learn what your treatment options are for this serious medical problem—the disease of obesity.
Well I thank you for listening and if you’d like more information you can check out our other blogs or come to our weight loss seminars. We have both surgical and nonsurgical weight loss seminars directed towards treating this disease.