Bariatric providers require patients to take a bariatric multivitamin after weight surgery, along with other vitamins, to ensure optimal health. After bariatric surgery, the digestive tract will be altered, reducing the amount of vitamins and minerals absorbed by the body. Therefore, to avoid malnutrition, patients will be required to take vitamins for life after their weight loss surgery procedure. Yet, choosing a bariatric multivitamin can become overwhelming. In this blog, we break down what you need to look out for when selecting a complete bariatric multivitamin.
Bariatric Multivitamins 101
The most vital supplement to take after weight loss surgery is a complete bariatric multivitamin. Multivitamins are a great way to get all the essential nutrients you may need after weight loss surgery without having your pantry overtaken by supplements. Still, how should you go about choosing your bariatric multivitamin, and what is it even made of? Let’s dive in.
Vitamin B12 (Cyanocobalamin and Methylcobalamin)
Recommended Dosage: 1000 mcg
B12 is one of the most common vitamin deficiencies after bariatric surgery. B12 is an essential nutrient for metabolic and nervous system health and helps break down fatty acids and amino acids to provide you with energy and strengthen your immune system.
Biotin (Vitamin B7)
Recommended Dosage: 600 mcg
Also known as the beauty vitamin, biotin is an essential nutrient for better hair, skin, and nails and helps support metabolic processes, which is essential after weight loss surgery.
B Vitamins (Vitamins B1, B2, B5, B6)
Recommended Dosage: 12 to 20 mg
The bariatric patient’s favorite vitamins, B1, B2, B5, and B6, are critical for healthy skin, hair, muscles, nervous system, and brain function. But, better yet, the B vitamins are essential in the process of converting carbohydrates into energy.
Vitamin A (from Beta Carotene & Vitamin A Acetate)
Recommended Dosage: 3,300 mcg
Vitamin A is used to form and maintain healthy teeth, bones, skin, and soft tissue.
Vitamin D (Calciferol)
Recommended Dosage: 75 mcg, 3,000 IU
The sunshine nutrient. A lack of vitamin D can cause bone deficiencies and other diseases. Vitamin D is required in high doses after bariatric surgery and is best absorbed with calcium, which is why there will also be vitamin D in most bariatric calcium supplements.
Chromium (as Chromium Picolinate)
Recommended Dosage: 100 mcg
Chromium is the insulin nutrient that helps maintain healthy blood glucose levels and converts glucose into energy, essential for patients with diabetes.
Vitamin E (as D-alpha tocopheryl succinate)
Recommended Dosage: 40.2 mg
An essential nutrient in wound healing, vitamin E aids in the production of red blood cells and assists vitamin K in the healing of wounds and scars.
Iron (from Ferrous Fumarate)
Recommended Dosage: 45 mg
Another common vitamin deficiency after bariatric surgery and the most probable reason for post-bariatric anemia, iron is essential in producing red blood cells and making amino acids.
Niacin (Vitamin B3)
Recommended Dosage: 40 mg
Otherwise known as vitamin B3, this nutrient helps maintain healthy skin, nerves, and brain and plays a vital role in lowering cholesterol levels.
Copper (from Copper Gluconate)
Recommended Dosage: 2 mg
Copper aids in metabolizing iron and supporting your immunity.
Folic Acid (L-Methylfolate Calcium)
Recommended Dosage: 800 mcg
Folic Acid is an essential nutrient in the production of DNA and vital for women of childbearing age as a lack of folate can result in birth defects.
Selenium (Selenium Amino Acid Chelate)
Recommended Dosage: 100 mcg
Selenium helps fight oxidative stress that could result in chronic health conditions such as heart disease and cancer. Low selenium levels in post-bariatric patients could result in cardiomyopathy.
Molybdenum (as Molybdenum Amino Acid Chelate)
Recommended Dosage: 75 mcg
Molybdenum is an essential mineral found in most grains and legumes. This nutrient helps break down unhealthy toxins in the body.
Zinc (Zinc Oxide and Zinc Amino Acid Chelate)
Recommended Dosage: 16 mg
Zinc is critical to the support of a healthy immune system and optimal metabolic control.
Vitamin C (L-ascorbic acid)
Recommended Dosage: 130 mg
The immunity mineral, vitamin C bolsters the immune system and plays a vital role in wound healing and the regeneration of antioxidants.
Vitamin K (Phytanadione)
Recommended Dosage: 120 mcg
Vitamin K is an essential nutrient in the blood clotting process and assists wound healing after bariatric surgery.
Iodine (as Potassium Iodide)
Recommended Dosage: 150 mcg
Iodine is a mineral essential to thyroid control by regulating your metabolism for weight and energy control. Iodine also promotes skin repair and slows down the appearance of aging—a woman’s best friend.
Manganese (as Manganese Sulfate)
Recommended Dosage: 2 mg
Manganese is essential in the formation of bones and helps metabolize amino acids, cholesterol, and carbohydrates.
Magnesium (as Magnesium Oxide, Magnesium Amino Acid Chelate & Magnesium Citrate)
Recommended Dosage: 100 mg
Magnesium is an essential mineral that aids in absorbing and breaking down the other ingredients in the vitamin formulation.
Bariatric Multivitamin Frequency
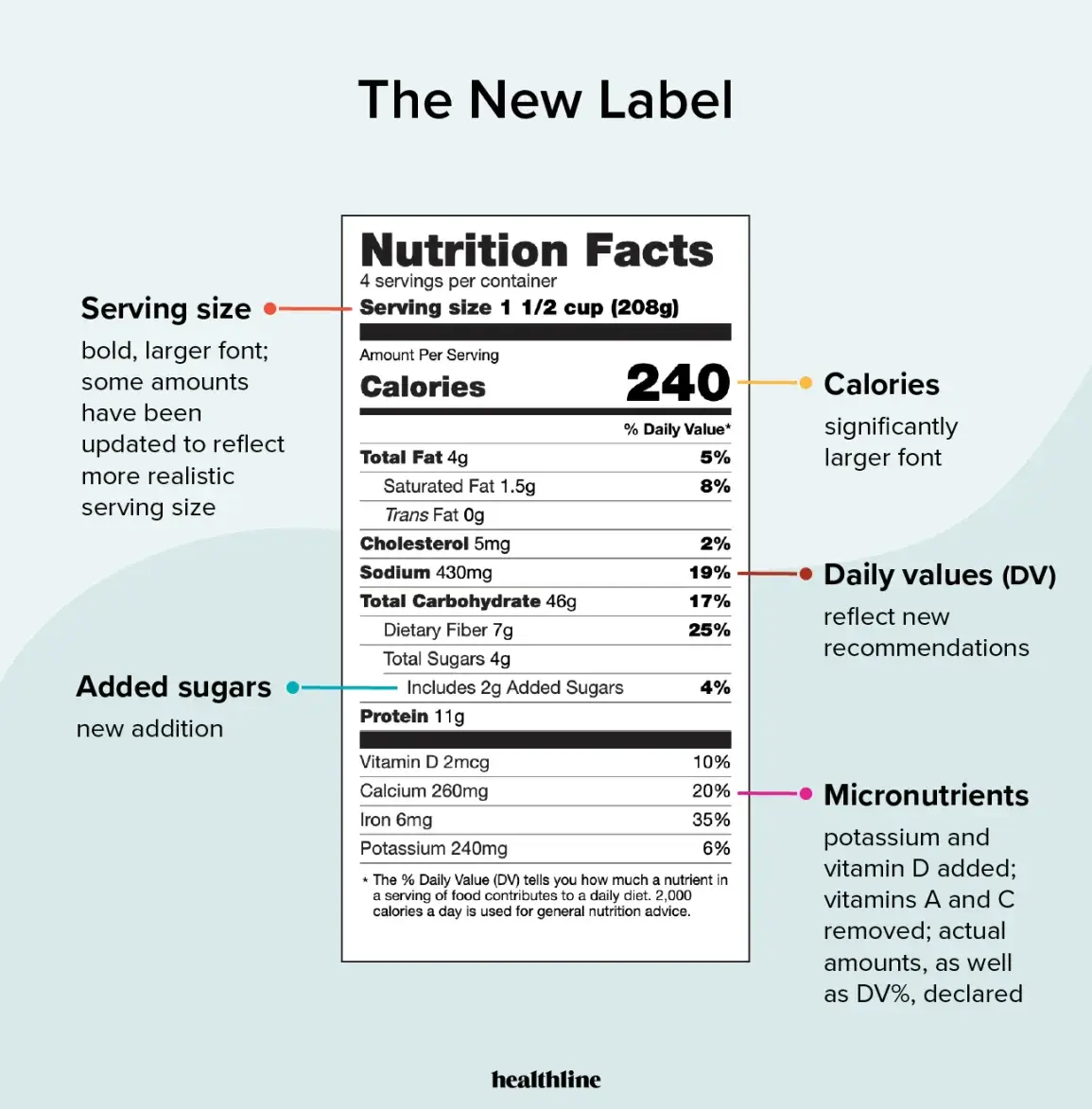
When purchasing a bariatric multivitamin from a reputable retailer, almost all of them will contain the recommended dosage of each mineral listed above. But we still recommend you thoroughly review the nutrition label to ensure you are getting the appropriate doses after your bariatric procedure. Bariatric multivitamins must be taken up to two times daily, depending on the brand of vitamin you are taking. If you have the Live Healthy MD Complete Bariatric Multivitamin, you only need to take one vitamin a day.
Additional Bariatric Vitamins Needed
Bariatric patients must also take a calcium citrate supplement. It is essential to remember to take calcium citrate, NOT the calcium carbonate supplements found at your local convenience store. Calcium carbonate is not absorbed as quickly as calcium citrate is. For patients who had the gastric bypass or the gastric sleeve, the recommended dosage is 1500 mg of calcium citrate per day. If you had the duodenal switch, you would be required to take 2000 mg per day.
There are several options on the market for bariatric supplements. Yet, no matter which brand you choose to take, be sure to review the nutrition label thoroughly to ensure the product you are buying has the recommended dosage of each vitamin and mineral. It is necessary to understand that bariatric multivitamins are very different from other complete multivitamins. If you have any questions regarding what vitamins to take after weight loss surgery, we encourage you to reach out to your bariatric care team.